Diabetic Retinopathy A Silent Threat to Vision
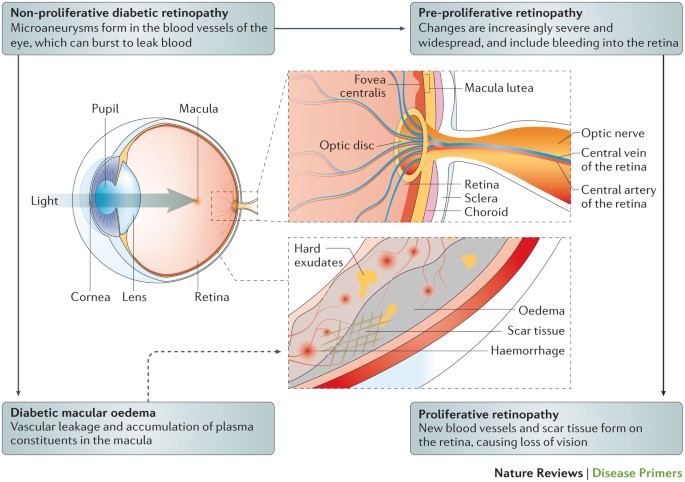
Diabetic retinopathy is a serious eye condition that can occur in people with diabetes. It’s caused by damage to the blood vessels in the retina, the light-sensitive tissue at the back of the eye.
What Happens in Diabetic Retinopathy?
High blood sugar levels can damage the tiny blood vessels in the retina. This damage can lead to:
- Microaneurysms: Tiny bulges in the blood vessels that can leak fluid or blood.
- Blocked blood vessels: Can deprive the retina of oxygen and nutrients.
- Abnormal blood vessel growth: New, fragile blood vessels can grow on the surface of the retina, leading to bleeding and scarring.
Symptoms of Diabetic Retinopathy
In the early stages, diabetic retinopathy often has no noticeable symptoms. However, as the condition progresses, symptoms may include:
- Blurred vision
- Floaters: Spots or streaks that appear to float across your field of vision.
- Dark spots in your central vision
- Difficulty seeing at night
Preventing and Managing Diabetic Retinopathy
To prevent or manage diabetic retinopathy, it’s important to:
- Control blood sugar levels: Regular monitoring and medication can help keep blood sugar levels in check.
- Regular eye exams: Regular eye exams can help detect early signs of diabetic retinopathy.
- Healthy lifestyle: A healthy diet, regular exercise, and quitting smoking can reduce the risk of complications.
- Laser treatment: Can help seal leaking blood vessels and prevent further damage.
- Vitrectomy: A surgical procedure to remove scar tissue and repair retinal damage.
Early detection and treatment are crucial for preventing vision loss due to diabetic retinopathy. If you have diabetes, it’s important to schedule regular eye exams to monitor your eye health.